Teledermatology is at the forefront of this digital health revolution, and First Derm uses innovation and quality healthcare to drive this revolution forward.
What is Teledermatology?
Lets start at the beginning! What is teledermatology anyway? Quite simply, it is dermatology online. If you have a skin rash or any skin concern for that matter, be it skin cancer or otherwise then you will need the help of a dermatologist. Teledermatology, is all of this but online.
Why is Teledermatology Important?
Put simply, healthcare in the US, is similar to other western countries. It is facing ever-increasing pressure and increased needs due to accommodate certain factors such as an aging population. Unfortunately, an increased demand for specialist care patients, is met with fewer resources, which inevitably leads to increased waiting times to see dermatologist (here you wait the longest to meet a dermatologist). Furthermore, both the number of time-consuming, unnecessary specialist consultations and cosmetic consultations increase.
The New Solution
At present, referrals from a primary care centre to a dermatologist are frequently done by a referral written on paper on behalf of the patient. This is then sent from the primary care centre to the nearest dermatology clinic either by traditional mail or by fax!
Telemedicine, supported by the WHO is defined as healthcare performed remotely through information and communication technologies (ICT, eg computers, internet, mobile phones, satellites, etc.)
In fact, research demonstrates (found below in this article) that is is equivalent to a face-to-face (FTF) physical consultation when it comes to diagnostic precision and reliability. In outpatient care, teledermatology has proven to be reliable and diagnostically reliable for a large number of dermatological conditions. Furthermore, it reduces waiting times, increase access, and improve patients’ satisfaction and quality of life.
As mentioned, several studies show that 18-42% of all unnecessary visits to a dermatologist can be avoided. This is due the high level of certainty that a dermatologist can make the right diagnosis in the referral assessment online. Furthermore, studies indicate that the primary care referrals can be halved or reduced by 68%.
Is Teledermatology Accurate?
Family doctors make the correct diagnosis of the most common skin diseases in about 50% of the time
Skin related disorders are common in primary care and amount to about 20% of all visits. Family doctors see patients with unclear skin diseases daily. Furthermore, skin diseases are often very difficult to diagnose properly by a non specialist.
Studies show that family doctors or internists diagnose the most common skin diseases correctly in about 50% of cases, while a dermatologist diagnoses correctly in 96% of cases. In case of poor communication between the family doctor and the referring dermatologist, patients may potentially be disadvantaged and receive inadequate treatment and a delayed diagnosis.
Fast? Some say too fast!
As mentioned earlier a teledermatology service like ours speeds things up. Not just for you but also for the hospitals, doctors and researchers. In fact we actually find our service is so fast that people became suspicious! Naturally as humans, it takes us a while to adjust to change. Teldermatology is no different. How can a check up be so quick and yet still be accurate?
Since the average wait time to schedule a dermatologist’s appointment is 32 days and patients typically spend 10-15 minutes in the waiting room before seeing a doctor. It is no surprise that we question a service that can resolve your issue within an hour.
Ultimately, Telehealth provides quicker access to health care and shorter wait times, but only about 30% of Americans know that online doctors exist and only 17% have tried it. The waiting room process is so ingrained in our brains that if you get an answer quickly, you think it’s too good to be true.
Fast and Accurate
Our teledermatology service prides itself as “the fastest way to ask a dermatologist” disrupting the long waiting process of our existing health care system. At First Derm, users get an answer from a dermatologist within 8 to 48 hours, sometimes even faster.
For most this is not really an issue, people will catch up, whats the problem?! Unfortunately for us, things are slightly different. We are often surprised and disappointed when we receive negative feedback from users because we answer queries in minutes instead of hours.
In fact, most of our negative feedback is from people who are so used to the long waiting process that they’re skeptical of the fast response.
Teledermatology Research
Below we take you through the journey of our Teledermatology service. How did we reach where we are today? Learn more below.
Today, our population faces serious health related threats as the baby-boomer generation becomes elderly, viruses such as Zika spread throughout the world, and chronic diseases such as cancer develop without a cure.
At the same time, technology advances means technology has found its way into the pockets of vast segments of our society through mobile devices. There is, therefore, an intersection between health related threats and accessible technology. This presents us with the perfect opportunity to improve the lives of many, at a fast rate. The digital health revolution can improve not only patient outcomes, but also the efficiency of our healthcare system. Teledermatology is at the forefront of this digital health revolution, and First Derm uses innovation and quality healthcare to drive this revolution forward.
The Beginning
The idea behind First Derm was not thought up overnight – it is the product of years of development and scholarly research. First Derm, was founded by Dr. Alexander Börve, a medical doctor and an academic in the field of teledermatology. Since 2008, he has published 4 peer-reviewed scholarly articles demonstrating the success of teledermatology:
- Smartphone Teledermoscopy Referrals: A Novel Process for Improved Triage of Skin Cancer Patients
- Mobile teledermoscopy-there’s an app for that!
- Use of the mobile phone multimedia messaging service for teledermatology
- A pilot study of a medical information service using mobile phones in Sweden
Academic research focusing on the impact and accuracy of teledermatology began in 2009 when Dr. Alexander Börve and his colleagues conducted a pilot study in Swedish primary care centers. This pilot study, driven by iDoc24 Inc., illustrated the convenience of an app which provides medical information services through a mobile device.
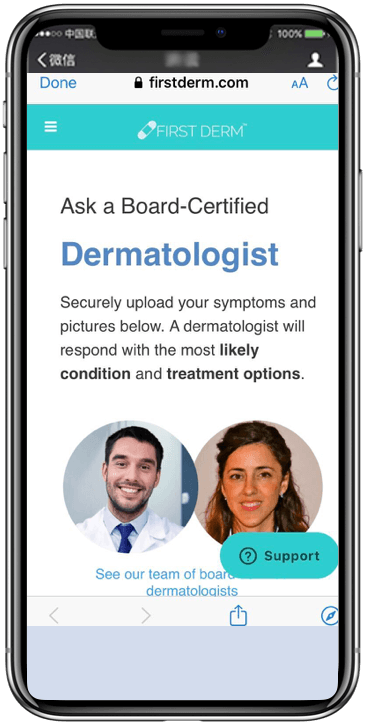
Individuals and/or physicians were able to take a picture of a skin ailment, send the picture anonymously to a dermatologist, and receive a response within 24 hours for an affordable price.1 Dermatologists provided the user with a suggested diagnosis and a recommended treatment. This business to consumer (B to C) model eventually developed into the First Derm app. Here, the consumer can download for free and anonymously (no registration or e-mail necessary) under HIPAA. Meanwhile, the business to business (B to B) model evolved into the iDoc24 PRO app, allowing healthcare professionals to register for an account with the app with HIPAA compliance.
From a Pilot To Comprehensive Research
Using the Tele-Dermis ® platform, the first study conducted by Dr. Börve was a small pilot of 51 patients referred from family doctors to dermatologists. In 80% of the cases, family doctors wanted a second opinion for suspected skin cancer lesions. In 90% of those cases, the dermatologist wanted to further inspect lesions with a dermoscope.2
With the remaining 20% of referrals that were not suspected to be (classified as) skin cancer, the family doctor did not need to send the patient to a dermatologist visit for further inspection. However, they were given a skin treatment recommendation.2 Furthermore, suspected skin cancer lesions were difficult to diagnose due to low image resolution of the cell phone camera. Fortunately, since this original study, life and technology has moved on. Smartphones have such high quality cameras that we haven’t had a problem with this since 2015!
Building on our studies: The Dermoscope | Dermatoscope
With the diagnostic accuracy to be comparable to face-to-face visits on suspected skin cancer lesions, teledermoscopy offers the patient less time waiting for a suggested diagnosis and treatment option.
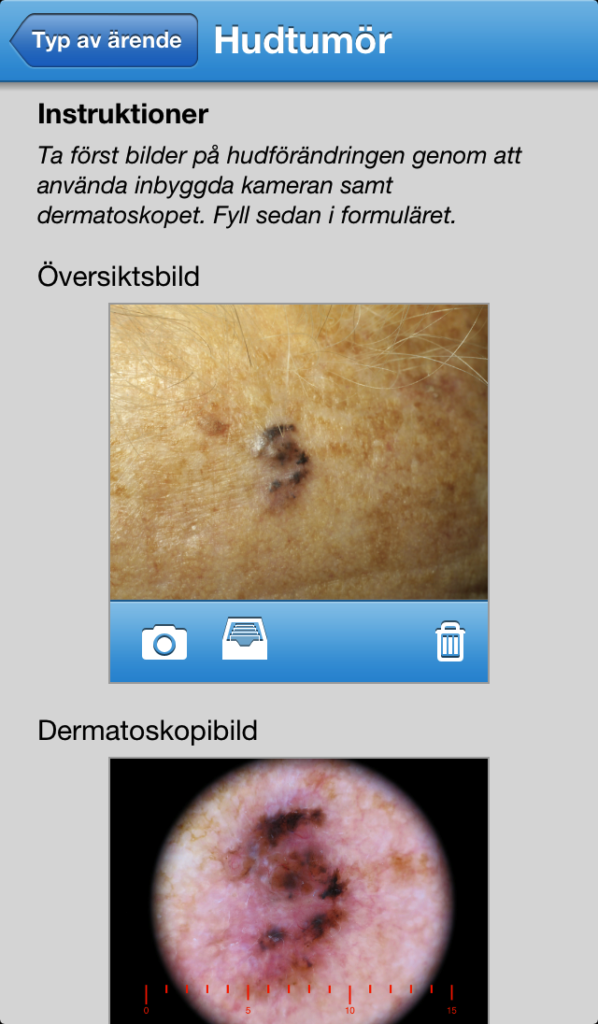
One of the first studies comparing teledermoscopy images and mobile images was done by Dr. Kroemer, an avid researcher and member of the Medical University of Graz teledermatology project. This mobile teledermatology study affirmed that the teledermoscopy images were superior when juxtaposed to standard mobile images.3 Following this study, the dermoscope was redesigned as an iPhone attachment, and Dr. Börve and his team further tested the accuracy this technology in their 2013 study, “Mobile teledermoscopy- there is an app for that!” Overall, this study confirmed the accuracy of teledermoscopy images and suggested that using the teledermoscopy image and the mobile image together would prompt a better dermatological response.4
Picture Quality an Issue No More
Each progressive study allowed Dr. Börve and his team to refine the methodology of teledermatology. The main flaw in early studies was the low picture quality to assess possible skin cancer lesions, which in turn affected the accuracy of diagnosis and triage decisions. This prompted the innovation of the dermoscope to improve accuracy across the board. Ironically, our Dermoscope is now less of a need due to the high quality cameras on smartphones.
Teledermoscopy has demonstrated a very comparable diagnostic accuracy to a face to face appointment with a dermatologist.4 With the diagnostic accuracy to be comparable to face-to-face visits on suspected skin cancer lesions. Equally, it provides the patient with less time waiting for a suggested diagnosis and treatment option. Furthermore, less time spent waiting means less time for the cancer to grow deeper into the skin.
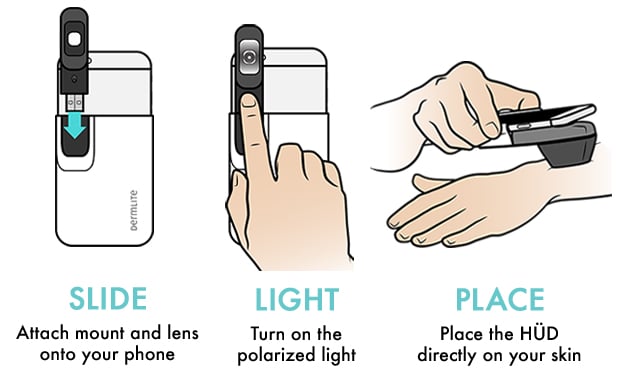
HÜD | Dermoscope (Dermatoscope)
As a result, 93% of patients in the sample had treatment on the first visit compared to 82% in the traditional referral method.
12,000 people die of skin cancer every year in the USA. Unlike most cancers, skin cancer has a very high survival rate if detected early enough. Studies from Australia show that education and proactive screening can save people from skin cancer deaths.
What is a Dermoscope?
A dermoscope is a magnifying glass with LED lighting that is used in everyday practice at a dermatology clinic. As a consumer, you can screen worrisome lesions that you think are potentially skin cancer and receive an opinion from a board certified dermatologist that is educated in reading dermoscopy images. Now we can perform this same test with a smartphone image, however, there is no denying the enhanced accuracy of the Dermoscope.
If you have more than 3 possible skin cancer lesions that you want to examine, we recommend that you see a dermatologist for a full body skin examination. Despite that, our service is well-suited to check one off lesions that may be worrying you between regular checkups. You can use the dermoscope on yourself, your partner, your parents or your kids.
Suspicious skin lesions were always very difficult to assess with only a smartphone camera. We’re not sure if you remember how bad they were but we do remember having a camera with 1.3 megapixel camera! With a dermoscope, such as HÜD, our scientific studies show results comparable with a face-to-face visit to the dermatologist.
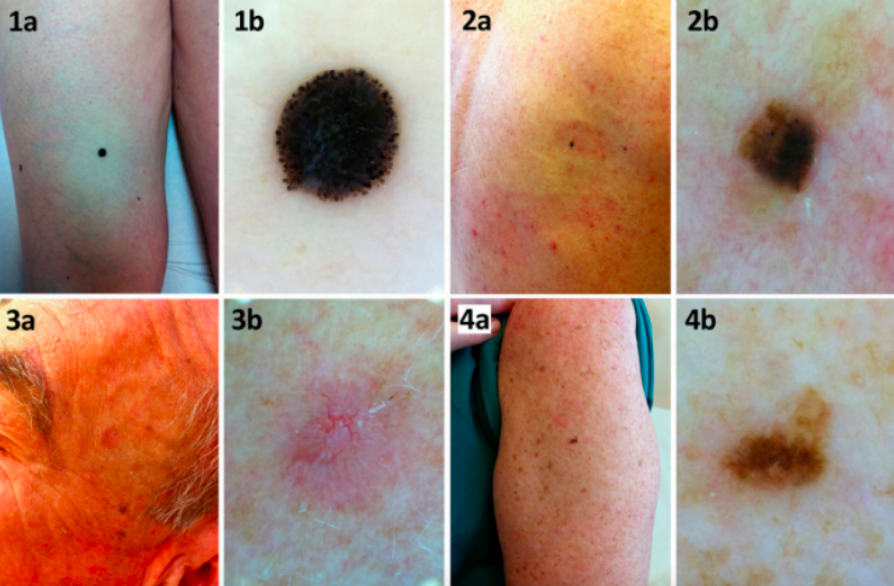
Images taken with a smartphone camera VS smartphone camera and dermoscope
Image quality of four different lesions included in the study. Clinical and dermoscopic images of (1a, 1b) a spitzoid nodular melanoma; (2a, 2b) a seborrheic keratosis; (3a, 3b) a basal cell carcinoma; and (4a, 4b) a dysplastic nevus. [Copyright ©2013 Börve et al.]¹
Further Studies
One of Dr. Börve’s latest studies connects family doctors with dermatologists by utilizing dermoscope technology with the iDoc24 PRO app platform. This pathway allows healthcare professionals that are not experts in dermatology to triage their patients prior to meeting a dermatologist. Especially those with suspected skin cancer concerns where time is of the essence.
This one-year study which included over 1500 patients, found that skin cancer lesions could be triaged to a dermatologist in an accurate, timely fashion. If properly used, this technology could save several weeks in referring the right patient at the right time for final diagnosis and treatment. As a result, 93% of patients in the sample had treatment on the first visit compared to 82% in the traditional referral method. Teledermatology can reduce 40% of dermatology clinic visits.5
Costs and Benefits
Telehealth, particularly teledermatology, can save the healthcare system several million dollars by accurately and time efficiently diagnosing and triaging patients.
To further explore the benefits of this technology, a cost-minimization report is being drafted to reveal the preliminary findings of First Derm. Telehealth, and specifically teledermatology, can save the healthcare system several million dollars by accurately and time efficiently diagnosing and triaging patients.
On a macroscopic scale, teledermatology has demonstrated a higher accuracy of triage referrals compared to paper referrals. Furthermore, this technology has the capacity to filter cases that can be managed outside the hospital for a fraction of the cost.
It is a technology designed to connect doctors with patients and provide pertinent medical information. On average there are about 3 dermatologist per 100,000 people in the US (fluctuating with population density).6 With this shortage of dermatologists, teledermatology and teledermoscopy provides a selective screening of cases currently unparalleled in our healthcare system. 70% of the cases First Derm receives are recommended over-the-counter medications and treatment, while only 30% are advised to seek a face-to-face visit.7 First Derm promotes a more efficient use of resources, time and money for doctors and patients via telehealth.
The Challenge of a Rising Population
Since our population is living longer, our healthcare system needs to evolve to serve more people more efficiently. A recent study estimates that 1 in 5 Americans will develop skin cancer within their lifetime, demonstrating the importance of diagnostic accuracy, triage management, cost and convenience.8 On average, primary care physicians only have an estimated 50% pretest examination and management accuracy of skin ailments, while teledermoscopists via First Derm are 90+% accurate and dermatologist face-to-face (FTF) are 98+% accurate.4,9 First Derm offers diagnostic accuracy comparable to a dermatologist FTF. Additionally, the technology enables swift triaging of patients through the convenience of a mobile phone.
The Future of Teledermatology
Ultimately, First Derm is efficiently and conveniently bridging the information gap between dermatologists and patients. Within hours accurate treatment recommendations and triage decisions are delivered to patients. First Derm is offering a research supported product employing accredited dermatologists that respond quickly to anonymous cases for an affordable price.
As technology evolves, features of this app has the potential to progress as well. Upgrading the dermoscope further will improve picture quality, in turn increasing the accuracy of dermatologists’ assessment. Even though technological advances shows promise for the future, all telehealth must overcome the slow-moving government policies. Plus the overall reluctance to change by doctors and the healthcare industry as a whole. In the face of adversity, First Derm is merging healthcare and technology to provide an efficient, convenient, and affordable product.
References
- Börve A., and R. Molina-Martinez. “A Pilot Study of a Medical Information Service Using Mobile Phones in Sweden.” Journal of Telemedicine and Telecare 15.8 (2009): 421-22. Web.
- Börve A., Holst A., Gente-Lidholm A, Molina-Martinez R., and Paoli J. “Use of the mobile phone multimedia messaging service for teledermatology.” Journal of Telemedicine and Telecare (2012): 18- 292. Web.
- Kroemer, S., J. Frühauf, T.m. Campbell, C. Massone, G. Schwantzer, H.p. Soyer, and R. Hofmann-Wellenhof. “Mobile Teledermatology for Skin Tumour Screening: Diagnostic Accuracy of Clinical and Dermoscopic Image Tele-evaluation Using Cellular Phones.” British Journal of Dermatology 164.5 (2011): 973-79. Web.
- Börve, A., Terstappen K., Sandberg C., and Paoli J. “Mobile Teledermoscopy—there’s an App for That!” Dermatology Practical & Conceptual 3.2 (2013): n. pag. Web.
- Börve A, Dahlén Gyllencreutz J, Terstappen K, Johansson Backman E, Aldenbratt A, Danielsson M, Gillstedt M, Sandberg C, Paoli J. “Smartphone Teledermoscopy Referrals: A Novel Process for Improved Triage of Skin Cancer Patients.” Acta Derm Venereol (2014). Web.
- Yoo, J. Y., and D. S. Rigel. “Trends in Dermatology: Geographic Density of US Dermatologists.” Archives of Dermatology 146.7 (2010): 779. Web.
- Buhr, Sarah. “An App That Detects STDs In The Privacy Of Your Own Home.” TechCrunch. TechCrunch, 19 June 2014. Web. 10 July 2014.
- Robinson, JK. Sun exposure, sun protection, and vitamin D. JAMA 2005; 294:1541-43.
- Ramsay, D. L., and A. B. Fox. “The Ability of Primary Care Physicians to Recognize the Common Dermatoses.” Archives of Dermatology 117.10 (1981): 620-22. Web.