Molluscum Contagiosum vs. Genital Herpes: How to Tell the Difference

Key Takeaways
| Characteristic | Molluscum Contagiosum | Genital Herpes |
| Cause | Poxvirus (MCV) | Herpes Simplex Virus (HSV) |
| Appearance | Pearly, dome-shaped with central dimple | Cluster of blisters or ulcers |
| Size | 2 to 6 mm | Variable |
| Texture | Smooth | Tender, fluid-filled |
| Pain | Painless | Painful |
| Symptoms | None specific to lesions | Itching, burning, flu-like symptoms |
| Area Affected | Anywhere on the body | Genital and anal areas |
Molluscum contagiosum (water warts) and genital herpes, both skin infections, are often confused due to their similar appearance. This confusion can lead to delayed treatment and mismanagement. Understanding the differences between these conditions is vital for accurate diagnosis and effective treatment. Both conditions have distinct characteristics that influence their management and treatment, as well as psychological impacts. This guide aims to clarify these differences to aid in better health decisions.
Overview of Molluscum Contagiosum & Genital Herpes
Molluscum Contagiosum
This is a viral skin infection caused by the molluscum contagiosum virus (MCV), a type of poxvirus. It typically appears as small, raised, painless bumps on the skin.

Molluscum Contagiosum : A Reddish-Whitish, Painless Papule or Lesion on the Penis Shaft
These lesions can develop anywhere on the body and are the primary indicator of the infection, which is usually mild. Genital lesions may resemble those of herpes or warts in their early stages but are distinct in being painless. Molluscum contagiosum is especially prone to rapid spread in individuals with weakened immune systems, like those with HIV/AIDS or severe eczema, making early recognition and management important[1].
Genital Herpes
This is a sexually transmitted infection (STI) primarily caused by herpes simplex virus type 2 (HSV-2).[2] It is characterized by painful sores in the genital and anal areas.
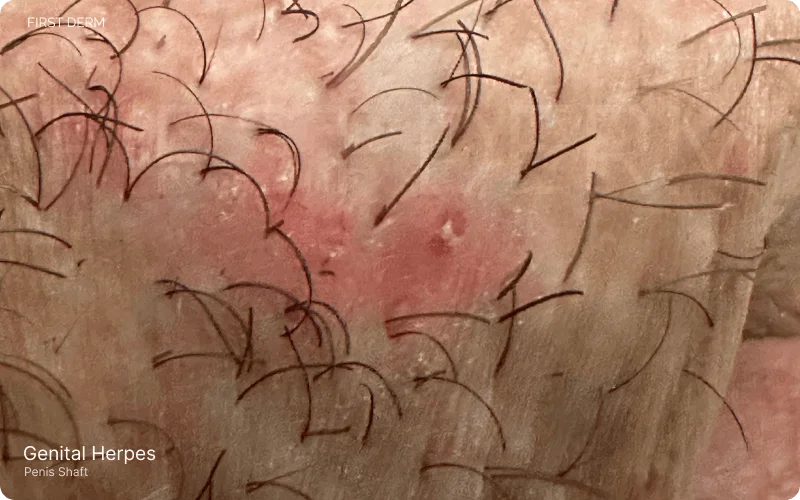
Genital Herpes on the Penis Shaft: Cluster of Small Blisters on Red, Inflamed Skin
Molluscum Contagiosum vs. Genital Herpes: Visual Differences and Causes
Molluscum Contagiosum present as small lesions ranging from 2 to 6 mm in size [3]. These growths are characterized by a small, flesh-colored, whitish, or pink hue and exhibit a distinctive appearance dome-shaped with a central dimple, resembling a tiny pimple. The lesions have a smooth surface, giving them a unique appearance. The painlessness of these lesions, coupled with their raised nature, sets them apart from other skin conditions.

Comparative View: Molluscum Contagiosum (Left) with Pearly, Dome-Shaped Blisters vs Genital Herpes (Right) with Itchy, Red-Inflamed Blisters
Genital herpes manifests as painful cluster of blisters or ulcers in the genital and anal areas [4]. These lesions are typically characterized by their tenderness, causing discomfort and irritation. The sores may be accompanied by other symptoms such as itching, burning sensations, and flu-like symptoms during initial outbreaks. The recurrent nature of these sores, triggered by various factors, adds complexity to their visual presentation
| Characteristic | Molluscum Contagiosum | Genital Herpes |
|---|---|---|
| Size | 2 to 6 mm | Varies |
| Color | Flesh-colored, whitish, or pink | Red inflamed skin around blisters |
| Shape | Pearly, dome-shaped with central dimple | Cluster of blisters or ulcers |
| Surface | Smooth | Varied (smooth/rough depending on stage) |
| Pain | Painless | Painful |
| Additional Symptoms | None specific | Itching, burning, flu-like symptoms |
Contrasting the visual characteristics of molluscum contagiosum and genital herpes reveals key differences. While molluscum contagiosum lesions are painless, small, and raised with a central dimple, genital herpes sores are notably painful, often accompanied by tenderness and flu-like symptoms. The color, texture, and overall appearance of these lesions provide essential visual cues for accurate identification,
Symptoms and Dormancy
Symptoms of Molluscum Contagiosum typically manifest after virus contraction, with the appearance of skin lesions being the primary indicator. Itchiness, inflammation, and swelling could be symptoms of the lesions. Initially, the bumps may be small and firm, but they may also be pink, white, or flesh colored. Most likely, these lumps will continue to grow. As the bumps expand, they take on a dome form and the indentation in the center can make it appear as pin into skin. Squeezing the lesion may also cause the infected person to observe the discharge of a wax-like substance. The virus that causes molluscum contagiosum can spread by close personal contact, including sexual contact, as it is a STI. The vaginal area is a common site for symptoms to manifest.
Pink eye is a common symptom of having a molluscum on your eyelid. When the molluscum contagiosum clears, the pink eye also tends to disappear. When the lumps turn red and resemble pimples, it is a sign that your immune system is working to eliminate the virus.[5]
The timing of symptoms varies, with some noticing the lesions shortly after exposure, while others may experience a delayed onset.
Genital herpes, known for its dormancy and recurrent nature, often presents with symptoms during outbreaks. Symptoms typically emerge 2 to 12 days after exposure to the virus and encompass pain or itching in the genital area, along with the appearance of small bumps or blisters near the genitals, anus, or mouth.[6] These blisters can rupture, resulting in painful ulcers that may ooze or bleed, forming scabs during the healing process. Other associated symptoms include painful urination and discharge from the urethra or vagina. The initial outbreak might also involve flu-like manifestations such as fever, headache, body aches, and swollen lymph nodes in the groin. The virus can then enter a dormant phase, with recurrent outbreaks triggered by various factors, leading to the reappearance of symptomatic sores.
Highlighting the symptomatic differences between molluscum contagiosum and genital herpes underscores the importance of accurate diagnosis. Molluscum contagiosum symptoms are primarily localized to the appearance of painless lesions, whereas genital herpes involves a more complex interplay of painful sores, flu-like symptoms, and the potential for recurrent outbreaks.[7] Understanding these distinctions is fundamental for individuals and healthcare professionals alike, guiding appropriate actions for effective management and care.
Transmission and Spread
How Molluscum contagiosum transmit & spread
- Transmitted through both sexual and non-sexual means.
- Sexual transmission: Direct person-to-person physical contact.
- Non-sexual transmission: Common among children.
- Contact with contaminated objects or surfaces (fomites), such as clothing, towels, bathing sponges, pool equipment, and toys.
- Possible transmission through shared towels and items in wet environments like swimming pools.
- Autoinoculation: Spreads to different body parts via touching or scratching a lesion.
- Spread facilitated by shaving and electrolysis.
- Virus confined to the epidermis, not transmitted through coughing or sneezing.
- Once lesions disappear, the virus is eradicated and cannot spread further.[8]
How Genital herpes transmits & spread
- Transmitted through vaginal, anal, or oral sex with an infected individual.
- Contact with a herpes sore, saliva (oral herpes), or genital fluids (genital herpes) can lead to transmission.
- Possible even if sores are not visible or the partner is unaware of their infection.
- Transmission via oral sex from someone with oral herpes.
- Cannot be contracted from toilet seats, bedding, swimming pools, or by touching objects like silverware, soap, or towels.
- Highlights the importance of informed precautions and safe practices.[9]
Diagnosis and Testing
Accurate diagnosis is crucial for effective management of Molluscum Contagiosum and Genital Herpes.
Diagnosing Molluscum Contagiosum
Diagnosing Molluscum Contagiosum often involves a thorough physical examination by a healthcare professional. The characteristic appearance of painless, raised lesions with a central dimple or crater is a key visual clue. In some cases, a biopsy may be performed, where a small sample of the lesion is taken for microscopic examination to confirm the presence of the molluscum contagiosum virus (MCV). While laboratory tests are not always necessary, they can provide additional confirmation in certain situations.[10]
Diagnosing Genital Herpes
Diagnosing Genital Herpes requires a combination of physical examination and laboratory tests. During a physical examination, healthcare professionals inspect the genital and anal areas for the characteristic painful sores associated with herpes. Laboratory tests play a critical role in confirming the diagnosis, typically involving the collection of swabs from the sores. Polymerase chain reaction (PCR) and viral culture tests are commonly employed to detect the presence of the herpes simplex virus (HSV) in these samples.[11] This comprehensive approach, combining visual examination and laboratory confirmation, ensures a more accurate diagnosis of Genital Herpes. Understanding the diagnostic methods for both conditions is fundamental in guiding appropriate treatment and management strategies.
Rapid Spread of Molluscum in Those with Weak Immune Systems and No Long-Term Effects Unlike Herpes
Molluscum contagiosum, a viral skin infection caused by the molluscum virus, poses a heightened risk of rapid spread in immunocompromised individuals, including those with HIV/AIDS or severe eczema.[14] Unlike herpes viruses, molluscum contagiosum lacks the potential for long-term herpes-like effects. The infection manifests as raised, pearl-like lesions and is prevalent in both the pediatric population and sexually active adults.
In immunocompromised cases, the ailment can persist for an extended duration and may lead to secondary bacterial skin infections. Preventive measures and prompt medical attention are crucial for immunocompromised individuals to mitigate the risk of complications.
Long-Term Effects of Molluscum Contagiosum in Those with Weak Immune Systems
Immunocompromised individuals affected by molluscum contagiosum face long-term consequences, marked by an elevated morbidity rate and a more extensive infection compared to their healthy counterparts. The primary concern lies in the potential development of secondary bacterial skin infections, necessitating timely treatment to curb further spread.[15] In contrast to herpes viruses, molluscum contagiosum does not exhibit a dormant phase with reappearance, emphasizing the significance of re-infection upon the emergence of new lesions. To address these long-term effects, immunocompromised individuals must prioritize seeking medical intervention and adopting preventive measures to minimize the associated risks and complications.
Prevention Tips for Molluscum Contagiosum and Genital Herpes
Molluscum Contagiosum
- Practice safe sexual practices, including using condoms, to reduce infection spread.
- Avoid close skin-to-skin contact, especially in the genital area, with infected individuals.
- Do not share personal items like towels, clothing, or toys that might carry the virus.
- Regular handwashing and maintaining good hygiene to lower infection risk.
- Seek medical advice for unusual skin lesions, especially in the genital area, for proper diagnosis and treatment.
Genital Herpes
- Consistent and correct use of condoms is advised, though it doesn’t offer complete protection.
- Open communication with sexual partners about herpes status and getting tested is vital. [17]
- Avoid sexual activity during outbreaks to reduce transmission risk.
- Seek medical advice if there’s suspicion of genital herpes or exposure to the virus.
- Educate oneself about symptoms and transmission to make informed sexual health decisions.
References
- Forbat E, Firas Al‐Niaimi, Ali F. Molluscum Contagiosum: Review and Update on Management. Pediatric Dermatology. 2017;34(5):504-515. doi:https://doi.org/10.1111/pde.13228
- World. Herpes simplex virus. Who.int. https://www.who.int/news-room/fact-sheets/detail/herpes-simplex-virus. Published April 5, 2023. Accessed November 14, 2023.
- Phelps A, Murphy MJ, Zendee Elaba, Hoss DM. Molluscum Contagiosum Virus Infection in Benign Cutaneous Epithelial Cystic Lesions—Report of 2 Cases with Different Pathogenesis? American Journal of Dermatopathology. 2010;32(7):740-742. doi: https://doi.org/10.1097/dad.0b013e3181d051bd
- Corey L, Adams HG, Brown ZA, Holmes KK. Genital Herpes Simplex Virus Infections: Clinical Manifestations, Course, and Complications. Annals of Internal Medicine. 1983;98(6):958-958. doi:https://doi.org/10.7326/0003-4819-98-6-958
- Hanson D; Diven DG. Molluscum contagiosum. Dermatology online journal. 2013;9(2). https://pubmed.ncbi.nlm.nih.gov/12639455/. Accessed November 14, 2023.
- Kaufman. Clinical features of herpes genitalis. Cancer research. 2023;33(6). https://pubmed.ncbi.nlm.nih.gov/4352381/. Accessed November 14, 2023.
- Cusini M, Massimo Ghislanzoni. The importance of diagnosing genital herpes. Journal of Antimicrobial Chemotherapy. 2001;47(suppl_1):9-16. doi:https://doi.org/10.1093/jac/47.suppl_1.9
- Bikowski JB. Molluscum contagiosum: the need for physician intervention and new treatment options. Cutis. 2017;73(3). https://pubmed.ncbi.nlm.nih.gov/15074350/. Accessed November 15, 2023.
- STD Facts – Genital Herpes. https://www.cdc.gov/std/herpes/stdfact-herpes.htm. Published 2023. Accessed November 15, 2023.
- Meza-Romero R, C. Navarrete-Dechent, Downey C. Molluscum contagiosum: an update and review of new perspectives in etiology, diagnosis, and treatment. Clinical, Cosmetic and Investigational Dermatology. https://www.semanticscholar.org/paper/Molluscum-contagiosum%3A-an-update-and-review-of-new-Meza-Romero-Navarrete-Dechent/43660cbeeb26dce540fcfec3c4557f7ba01fd699. Published 2019. Accessed November 15, 2023.
- Cusini M, Massimo Ghislanzoni. The importance of diagnosing genital herpes. Journal of Antimicrobial Chemotherapy. 2001;47(suppl_1):9-16. doi:https://doi.org/10.1093/jac/47.suppl_1.9
- Treatment Options. https://www.cdc.gov/poxvirus/molluscum-contagiosum/treatment.html. Published 2023. Accessed November 15, 2023.
- Gupta R, Wald A. Genital herpes: antiviral therapy for symptom relief and prevention of transmission. Expert Opinion on Pharmacotherapy. 2006;7(6):665-675. doi:https://doi.org/10.1517/14656566.7.6.665
- Bates C, Carey P, Dhar J, Hart CA. Molluscum contagiosum—a novel presentation. International Journal of Std & Aids. 2001;12(9):614-615. doi:https://doi.org/10.1258/0956462011923679
- Lin HY, Linn G, Liu C, Chen C, Yu KJ. An Immunocompromised Woman with Severe Molluscum Contagiosum That Responded Well to Topical Imiquimod. Journal of Lower Genital Tract Disease. 2010;14(2):134-135. doi:https://doi.org/10.1097/lgt.0b013e3181bf1a50
- Zichichi L; Maniscalco M. The challenges of a neglected STI: Molluscum contagiosum. Giornale italiano di dermatologia e venereologia: organo ufficiale, Societa italiana di dermatologia e sifilografia. 2013;147(5). https://pubmed.ncbi.nlm.nih.gov/23007250/ Accessed November 15, 2023.
- Handsfield HH. Public health strategies to prevent genital herpes: Where do we stand? Current Infectious Disease Reports. 2000;2(1):25-30. doi:https://doi.org/10.1007/s11908-000-0084-y
Ask a Dermatologist
Anonymous, fast and secure!

Dr. Raquel Molina Martinez is a board-certified dermatologist from Barcelona with over a decade of experience. Trained at Gothenburg’s University Hospital, she now practices at Centre Medic in Catalonia.

