Merkel Cell Carcinoma: Jimmy Buffett’s Rare Skin Cancer: What You Need to Know
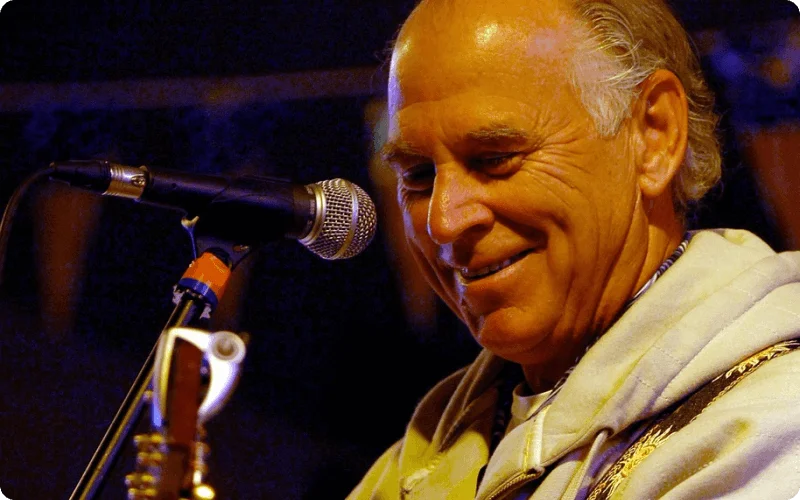
Jimmy Buffett has long been associated with a carefree lifestyle in music and entertainment. Merkel Cell Carcinoma was his biggest opponent behind the scenes. This rare and dangerous skin cancer took one of our favorite musicians and highlights the significance of understanding its severity. This article explores MCC, its rarity, and its potential effects, highlighting a worthy issue.
What is Merkel Cell Carcinoma (MCC)?
Merkel Cell Carcinoma (MCC) is an uncommon and severe form of skin cancer that originates from Merkel cells. Merkel cells are specialized skin cells that are predominantly responsible for touch sensation. These specialized cells are located in the epidermis and play a vital role in transmitting signals to the brain regarding tactile sensations.
MCC develops when Merkel cells endure malignant transformation, resulting in the formation of tumors. This transformation is frequently initiated by exposure to ultraviolet (UV) radiation from the sun or other sources. MCC is categorized as a neuroendocrine carcinoma due to its origin from neuroendocrine cells such as Merkel cells and its ability to produce hormones.
Nature of Merkel Cell Carcinoma (MCC)
Merkel Cell Carcinoma typically manifests on the skin as a firm, harmless, and rapidly growing nodule. These nodules are distinguished by their flesh-colored, red, or bluish-red hues. MCC is distinguished by its propensity for rapid dissemination. Merkel cells can rapidly invade adjacent tissues and lymph nodes, necessitating prompt diagnosis and treatment.
Comparative Analysis with Other Skin Cancers
In medical terminology, “carcinoma” refers to a malignant tumor composed of epithelial cells. However, what sets MCC apart is its neuroendocrine nature, distinguishing it from more common skin malignancies like basal cell carcinoma and squamous cell carcinoma. This singularity contributes to the rarity of MCC, making a comprehensive understanding of this condition essential.
By understanding the complexities of Merkel Cell Carcinoma, we can better comprehend the difficulties it presents and the significance of early detection and treatment. In the following sections, we will delve deeper into the causes, risk factors, and symptoms of MCC in order to provide you with a thorough understanding of this rare type of skin cancer.
Merkel Cell Carcinoma-Epidemiology and Statistics
Why rare disease?
Merkel Cell Carcinoma (MCC) is rare due to its low prevalence. This rarity is highlighted by its, 1 case per every 130,000 US cases. Compared to melanoma, MCC is 40 times rarer. The epidemiology of MCC explains its rarity.
Annual US MCC Case Estimates
Approximately 3,000 MCC cases are detected annually in the US. These numbers are expected to rise to 3,250 cases per year by 2025. This frightening trend is largely due to Baby Boomer aging. MCC incidence rates climb exponentially with age, highlighting the need for greater MCC diagnosis and management knowledge, especially given the constantly changing therapeutic landscape, according to (Paulson, 2017).
MCC vs. Melanoma
The fact that MCC is 40 times rarer than melanoma emphasizes its rarity. Both MCC and melanoma are skin cancers, although their risk factors and features differ. MCC risk factors include sun exposure, pale skin, age over 70, and impaired immune system. Baseline imaging has shown occult metastatic MCC at a higher rate than melanoma in clinically node-negative patients, stressing the necessity of early discovery and diagnosis (Singh, 2020).
More epidemiological insights:
- MCC mostly affects elderly white males’ heads and necks.
- MCC risk factors include UV exposure, aging, and immunosuppression.
- MCC is linked to Merkel cell polyomavirus infection.
- Understanding Merkel Cell Carcinoma epidemiology is essential to understanding its uncommon but violent skin cancer and the need of early detection and care.
Worried About a Skin Spot or Growth That Might be Cancerous?
Let a board-certified dermatologist evaluate your concern online. Confidentiality Assured: Share your symptoms and photos discreetly.
Merkel Cell Carcinoma Symptoms: Early Detection Is Key
Merkel Cell Carcinoma (MCC), although rare, is invasive and warrants attention. To effectively fight this skin cancer, you must detect its modest but substantial symptoms, comprehend MCC nodule visual clues, and understand why contacting a dermatologist at the first sign of probable symptoms is crucial.
Initial Symptoms
Specific visual cues help identify MCC nodules. These nodules are usually less than 2 centimeters wide, but their size might vary. Sun-exposed parts like the face, neck, and arms get them. Because MCC is unexpected, these nodules might appear anywhere on the body. Their fast growth and occasional ulceration or bleeding identify them.
Consult a Dermatologist for Potential Symptoms
Why Early Detection of Skin Cancer is Important?
Early detection is key to fighting skin cancer. Early skin cancer treatment, including MCC, is more effective and less intrusive. This can increase cure rates and reduce cancer spread.
Key to Early Detection the American Cancer Society advises
The American Cancer Society advocates skin cancer screening. Screening tests advised by the society can detect malignancies early. These screenings are important and timed according to risk factors, age, and medical history. These screenings may be covered by insurance.
Most Safe Way to Detect Skin Cancer
Dermatologists can safely diagnose skin cancer, including MCC, through frequent skin exams. These professionals can spot concerning lesions and biopsies.
How is early MCC treated?
Early-stage MCC requires surgery and biopsy. The surgeon removes the tumor and a margin of normal skin during surgery. Lymph node dissection may be done if the malignancy has spread to neighboring lymph nodes.
Overall, Merkel Cell Carcinoma identification requires conscientious observation and timely dermatologist consultation. Recognizing the modest but specific symptoms, appreciating the need of early discovery, and following the American Cancer Society’s screening recommendations will improve the chances of controlling this rare but potentially invasive skin cancer.
Diagnosis and Staging of MCC
Merkel cell carcinoma diagnosis
Merkel Cell Carcinoma (MCC) diagnosis requires a comprehensive approach. Early detection improves outcomes and usually entails several steps:
The Diagnosis of MCC:
Full-Body Skin Exams:
Skin exams are generally the first step towards early detection. Dermatologists check skin for MCC-related growths, nodules, and blemishes.
Biopsies:
Biopsies are best for diagnosis. A biopsy takes a tiny tissue sample from the suspected MCC lesion. Pathologists check this tissue for MCC characteristics under a microscope.
Correct and Reliable Diagnostics:
The most accurate and reliable diagnostic methods for early Merkel Cell Carcinoma detection involves several methods,
Dermoscopy: This non-invasive method magnifies skin lesions with a handheld tool to distinguish MCC from benign growths.
Immunohistochemistry: Pathologists use immunohistochemistry to find MCC markers and confirm the diagnosis.
Advanced Imaging Methods:
Advanced imaging can help stage MCC. Methods include:
- PET-CT (Positron Emission Tomography-Computerized Tomography): PET-CT scans show MCC levels in the body, aiding staging.
- MRI scans can assess MCC in soft tissues, including tumor size and involvement.
Sentinel Lymph Node Biopsy:
Sentinel lymph node biopsy is a routine MCC method that accurately determines lymph node status.
Biological and genetic markers:
Research is ongoing on biomarkers and genetic markers for diagnosis and prognosis. These markers may help MCC patients receive targeted treatment.
Understanding TNM Staging for Merkel Cell Carcinoma
Before discussing treatment choices, we have to understand the TNM staging method, which classifies MCC by tumor size (T), lymph node involvement (N), and metastasis(M).
The following parameters classify MCC:
T: Primary tumor
- TX: Primary tumor size is unmeasurable.
- T0: No primary tumor found.
- T1, T2, T3, T4: Primary MCC tumor size and extent. Higher T numbers indicate larger or more invasive tumors, with T3a and T3b providing more detail.
N: Regional Lymph Nodes
- The presence of MCC in surrounding lymph nodes cannot be accurately measured.
- N0: No adjacent lymph nodes show MCC.
- N1, N2, N3: MCC-containing lymph nodes’ number and position. Higher N numbers indicate more MCC-affected lymph nodes.
M: Metastasis Width
- MX: MCC metastasis is unmeasurable.
- M0: MCC has not spread.
- M1: MCC has spread.
The TNM staging system helps determine Merkel Cell Carcinoma’s severity. It guides treatment and gives patients prognostic information. Healthcare providers use TNM staging to accurately assess MCC patients. This standard method ensures MCC stage reporting accuracy.
In-depth examination of the various treatments according to stage
Surgical Removal (Treatments for T-Stage):
Surgical removal is the main treatment for T1-T2 MCC. This involves removing the tumor and a healthy margin that ensures total removal. This method has great success rates, especially for confined cancers.
Advanced Stages Chemotherapy:
In severe situations, chemotherapy may be suggested if MCC has progressed to lymph nodes or distant organs (N1-M1). Powerful medications target cancer cells throughout the body in chemotherapy. The patient’s stage and health determine effectiveness.
Adjunct or Primary Radiation Therapy:
After surgery, radiation therapy is used to kill remaining cancer cells or as a primary treatment for patients who cannot have surgery. Stages with higher success percentages have different outcomes.
Immunotherapy (Cutting-Edge)
Immunotherapy for MCC is promising. It uses the immune system to combat cancer. Immunotherapy gives MCC patients hope, but results and side effects differ.
Lymph Node Dissection for Spreading Cancer
If MCC has spread to surrounding lymph nodes, dissection may be advised. This surgery removes lymph nodes, helping manage disease and plan treatment.
Can Early-Caught MCC Be Cure?
MCC is treatable if found early, especially in T1 and T2. Early diagnosis and treatment greatly boost remission chances.
Can MCC Return After Two Years?
Even after treatment, MCC can return. Regular follow-up checkups are essential to detect recurrence, especially in the first few years after therapy.
Health and Age-Related Treatment Variations
The patient’s age and health may affect MCC treatment. Individualized treatment strategies balance efficacy and tolerability.
New and Experimental Treatments
Novel immunotherapies and targeted therapeutics for MCC are being studied. These therapies may be beneficial but carry dangers that must be considered.
Long-term outlook
Stage, treatment, and individual characteristics affect MCC patients’ long-term prognoses. Early detection and treatment improve outcomes. MCC therapy options vary by disease stage. Early detection ensures the best results. Regular follow-up care is needed to detect recurrence and explore new treatments.
References
Graboski, J. S. (2008). A Comparison of Merkel Cell Carcinoma and Melanoma:Results from the California Cancer Registry. Clinical Medicine, 2, 327-333.
Paulson, K. P. (2017). Merkel Cell Carcinoma: US frequency and potential demographic trends. Journal of the Amerrican Academy of Dematology, 78, 457 – 463.
Singh, N. A. (2020). Clinical Benifits of Baseline Imagine in Merkel Cell Carcinoma. American Academy of Dermatology Journal., 584.
Ask a Dermatologist
Anonymous, fast and secure!

The Specialist doctor from the University Hospital in Gothenburg, alumnus UC Berkeley. My doctoral dissertation is about Digital Health and I have published 5 scientific articles in teledermatology and artificial intelligence and others.

