Vulvitis
Medically reviewed by The Dermatologists and written by Dr. Alexander Börve
- Requires medical diagnosis
- Symptoms: Extreme and constant itching, small cracks, sores, blisters or scaly and thick patches
- Color: Typically red or whitish
- Location: On the vulva (the area of skin outside of the female genitalia) or labia (lips of the vagina)
- Treatment: Anti-fungal creams, hydrocortisone creams, prescription sitz baths with soothing or topical estrogen cream
ICD-9: 616.0
Last updated on February 12, 2024
What is Vulvitis
Vulvitis is not a disease, but an inflammation of the vulva caused by an infection, allergy or injury. The vulva is the area of skin outside of the female genitalia, and is prone to irritation because of its moistness and warmth.
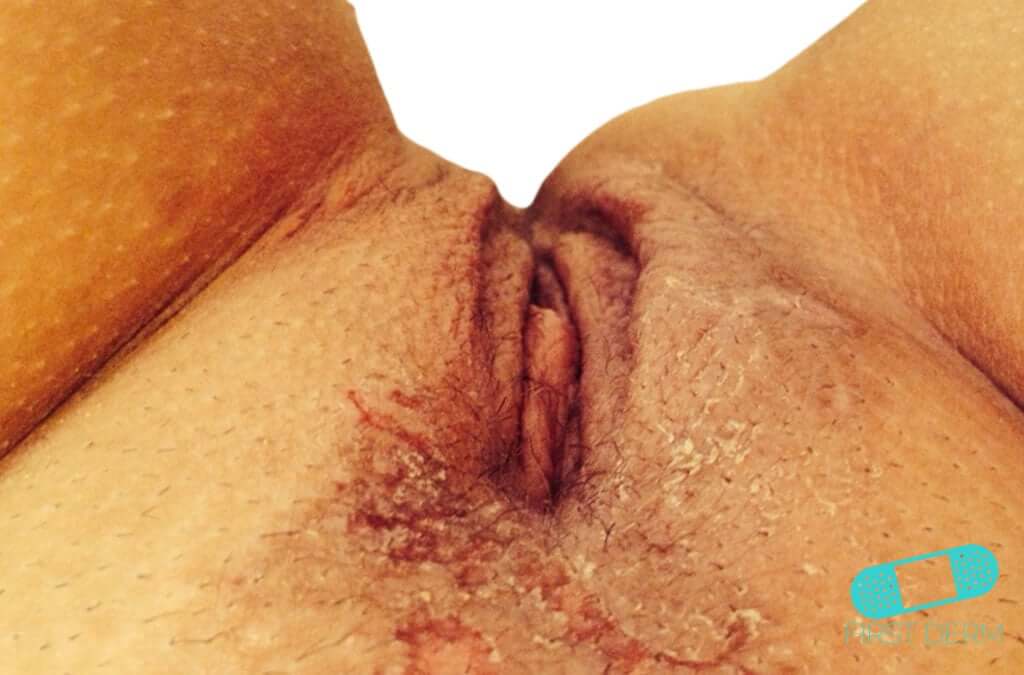
vulvitis: a condition involving inflammation of the vulva, characterized by symptoms such as redness, swelling, and irritation.
Some irritants that cause vulvitis are vaginal sprays, fungal infection, and dermatitis. Stress, poor nutrition, and poor hygiene can also increase susceptibility.
Any woman of any age can be affected by vulvitis, especially those who have not yet reached puberty or are post-menopausal.
This susceptibility is largely due to lower estrogen levels in these groups, which result in thinner, dryer vulvar tissues, increasing the risk of irritation and inflammation.
Try our FREE dermatology search engine and get peace of mind within a second
Difference between vulvitis and vaginitis
Vulvitis specifically refers to inflammation of the vulva, the external genital organs, while vaginitis is the inflammation inside the vagina. When both conditions occur together, it is known as vulvovaginitis, encompassing a broader area of inflammation.
Symptoms of Vulvitis
Symptoms of vulvitis may include:
- Extreme and Constant Itching: Persistent itching in the vulva area, often described as severe and unrelenting.
- Small Cracks on the Skin: The appearance of tiny fissures or cracks on the skin of the vulva.
- Sores and Blisters: Formation of sores or blisters, which may burst and ooze.
- Scaly and Thick Whitish Patches: Development of thick, whitish patches on the skin of the vulva that feel scaly to the touch.
- Redness and Swelling: Redness and swelling affecting both the vulva and labia (the lips of the vagina).
- Vaginal Discharge: Presence of vaginal discharge, which can vary in consistency and color.
- Burning Sensation: A burning sensation in the affected area, contributing to discomfort.
Causes & what can I do?
Stop using the products that may be causing the inflammation in the vulva. Over-the counter cortisone creams may help reduce the irritation and itching.
To prevent inflammation in the vulva, you can use gentle, unscented cleaning products. Make sure to dry the genital area thoroughly after bathing. Maintaining genital hygiene and wearing loose, breathable clothing can also help. Long-term dermatitis or infections, such as pubic lice or mites (scabies), can also lead to vulvitis.
Avoid the following products/activities, which may cause vulvitis:
- Toilet paper with perfume or dye
- Soaps or bubble baths with perfume
- Shampoos and hair conditioners
- Laundry detergents
- Vaginal sprays, deodorants, and powders
- Spermicides
- Douching
- Hot tub and swimming pool water
- Underwear made of synthetic material without a cotton crotch
- Rubbing against a bike seat
- Wearing a wet bathing suit for a long period
- Injury from activities like cycling or horseback riding.
Beyond external irritants, vulvitis can be triggered by fungal or bacterial infections, viral conditions like genital herpes, and skin conditions such as eczema or dermatitis.
Try our FREE dermatology search engine and get peace of mind within a second
Should I seek medical care?
The symptoms of vulvitis can also suggest other disorders or diseases of the genitals. Contact a healthcare provider for more medical advice if you experience the symptoms of vulvitis.
A physician can then perform a full pelvic exam and check for vagina discharge for any infections. A urine sample is usually taken to rule out more serious causes of genital irritation (e.g. vulvar cancer) and sexually transmitted infections (STIs).
A comprehensive diagnostic approach may include a review of your medical history, a detailed physical examination, and specific tests such as urine and blood tests, STI screenings, and a Pap smear to accurately identify the cause of inflammation.
Treatment for Vulvitis
Anti-fungal creams and hydrocortisone creams help reduce the inflammation. Prescription sitz baths with soothing compounds and topical estrogen cream may also help reduce the symptoms of vulvitis.
For more targeted treatment, especially in cases where initial approaches do not provide relief, healthcare providers may explore additional tests to rule out conditions like lichen sclerosus or explore the need for more specialized treatments.
Try our FREE dermatology search engine and get peace of mind within a second
Prognosis and Living With Vulvitis
The prognosis for vulvitis is generally excellent, with most individuals seeing significant improvement within a few weeks of starting treatment. Living with vulvitis involves ongoing vulvar care and regular consultations with your healthcare provider to manage symptoms and prevent recurrences.
References
van Schalkwyk J, Yudin MH; INFECTIOUS DISEASE COMMITTEE. Vulvovaginitis: screening for and management of trichomoniasis, vulvovaginal candidiasis, and bacterial vaginosis. J Obstet Gynaecol Can. 2015;37(3):266-274. doi:10.1016/S1701-2163(15)30316-9
Woelber L, Prieske K, Mendling W, Schmalfeldt B, Tietz HJ, Jaeger A. Vulvar pruritus-Causes, Diagnosis and Therapeutic Approach. Dtsch Arztebl Int. 2020;116(8):126-133. doi:10.3238/arztebl.2020.0126
Johns Hopkins Medicine. Vulvitis. Available at: https://www.hopkinsmedicine.org/health/conditions-and-diseases/vulvitis.
Ask a Dermatologist
Anonymous, fast and secure!

The Specialist doctor from the University Hospital in Gothenburg, alumnus UC Berkeley. My doctoral dissertation is about Digital Health and I have published 5 scientific articles in teledermatology and artificial intelligence and others.

