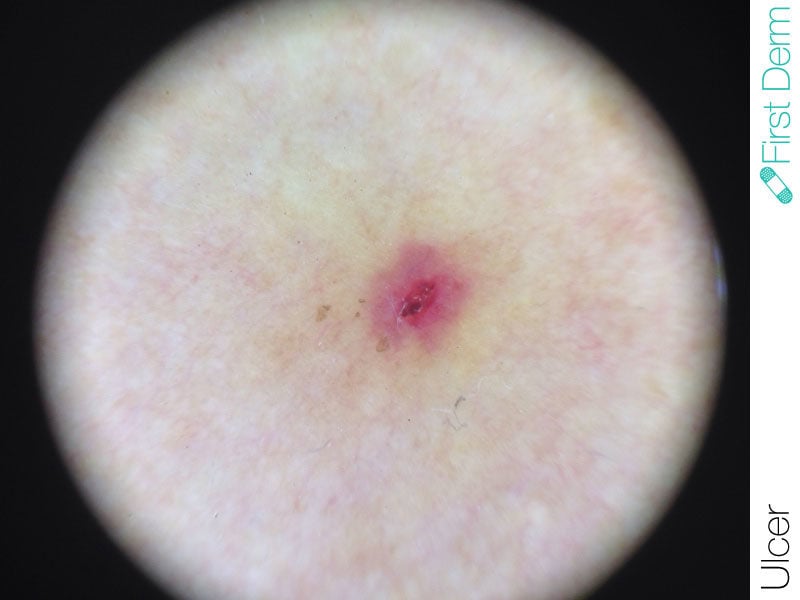
Ulcer
Medically reviewed by The Dermatologists and written by Dr. Alexander Börve
- Requires medical diagnosis
- Symptoms: Crater-shaped lesions surrounded by swollen skin, pain, discharge
- Color: Typically red
- Location: Anywhere on the skin
- Treatment: Metronidazole tablets and ointment, wet dressings, topical steroid creams and ointments or oral antibiotics
ICD-10: L88-L89
ICD-9: 707.00
An ulcer is a skin sore that appears red and is filled with pus upon infection. It can be triggered by excessive heat or cold, skin irritation, or problems with blood circulation.
Symptoms
Ulcers have a crater shape and are surrounded by red, swollen skin. They can be painful and produce discharge. Ulcers can have different causes, so it is important to know which type of ulcers you have for effective treatment.
Leg ulcer (Venous ulcer or stasis dermatitis)
Leg ulcer is caused by venous insufficiency, which leads to fluid and blood cells leaking from the veins into the skin and other tissues. Over time, this develops into permanent skin thickening and hardening and a bumpy, dark brown appearance on the legs’ skin. Skin ulcers then form, most commonly on the inside of the ankle.
Malignant skin ulcers
A skin ulcer occurs where an area of skin has broken down and you can see what lies underneath it (the underlying tissue). It is usually caused by a cancerous tumor on top of or just below the skin. It may produce discharge and bleed. If it becomes infected, it may cause an unpleasant smell.
Decubitus Ulcers (Bedsores or pressure sores)
Bedsores are caused from a lack of blood flow and from stress to the skin and tissues. They are classified into stages of severity by the National Pressure Ulcer Advisory Panel (NPUAP):
Stage 1: Skin is unbroken
- Pink or reddened
- May look like a mild sunburn
- Skin may be tender, itchy or painful
Stage 2: Upper layers of skin begin to die
- Red, swollen and painful skin
- Blisters that may be broken or intact
Stage 3: Sore has broken through the skin and wound, extends down to deeper layers of skin tissue
- Crater-like ulcers
- Prone to infection
Stage 4: Sore extends past the skin and into fat, muscle and bone tissue
- Blackened dead tissue (called “eschar”)
- Deep opened wounds
Unstageable: Sore has developed extensive damage to tissue layers
- Yellow or green ulcer
- Soft and look like pus
- Brown scab covering
Tropical ulcer
Tropical ulcer is also called tropical phagedaenic (phagedenic) ulcer. This is a painful, rapidly enlarging sore. It is usually found on the lower limbs of individuals living in a hot, humid tropical region.
Aphthous ulcer
Aphthous ulcers are typically recurrent round or oval sores or ulcers inside the mouth on areas where the skin is not tightly bound to the underlying bone, such as on the inside of the lips and cheeks or underneath the tongue. They can also affect the genitalia in males and females.
Try our FREE dermatology search engine and get peace of mind within a second
What can I do?
Prevention is different for different types of ulcer.
For leg ulcers, you may try elastic or compression stockings and avoid standing or sitting for long periods of time to reduce swelling in the lower legs. Avoid topical antibiotics, drying lotions, lanolin, benzocaine and other skin numbing agents, as they can make the problem worse.
For malignant skin ulcer, you may clean the ulcer with warm tap water and dress it special charcoal dressings. Avoid antiseptic washes, as it may be harmful to the tissues and thus delay healing.
For decubitus ulcer, correcting malnutrition, daily inspection of immobile person’s skin, frequent repositioning of immobile person and powered alternating-pressure mattresses can be helpful.
Should I seek medical care?
Recurrent aphthous ulcers are associated with significant health problems in some people. This includes Behcet syndrome, celiac disease, inflammatory bowel disease, human immunodeficiency virus (HIV) infection.
Treatments are very different for the various types of ulcers. Talk to a healthcare professional to outline a treatment plan for you.
Try our FREE dermatology search engine and get peace of mind within a second
Treatment
Antibiotics help prevent infection, but ulcers take a long time to heal. A healthy diet and exercise are important in preventing ulcers.
For leg ulcers, a healthcare provider normally suggests wet dressings, topical steroid creams and ointments or oral antibiotics to reduce the symptoms. Varicose vein stripping and other surgical procedures may be needed as well.
Metronidazole tablets and ointment can reduce unpleasant smell for malignant skin ulcers.
For decubitus ulcer, antibacterial drugs and “debridement” treatment can clear up the wound. However, ulcers past stage 2 are very difficult to treat.
Source:
US Skin Disease Assessment: Ulcer and Wound Care. Alina Markova, Eliot N Mostow Dermatol Clin. 2012 Jan;30(1):107-11
Ask a Dermatologist
Anonymous, fast and secure!

The Specialist doctor from the University Hospital in Gothenburg, alumnus UC Berkeley. My doctoral dissertation is about Digital Health and I have published 5 scientific articles in teledermatology and artificial intelligence and others.