Cercarial Dermatitis (Swimmer’s itch)
- More frequent during the Summer months
- Allergic reaction: Due to parasites called Schistosomes
- Symptoms: Rash with reddish pimples & itching or burning | Rash may progress into blisters in 2 or 3 days, and may rupture due to scratching or rubbing
- Location: Usually appears in places where the skin was directly exposed to contaminated water (such as the arms, legs, or torso)
- Typically lasts for a week or less and then fades away
- ICD: B65.3
You can find swimmer’s itch just about anywhere in the world because of its global distribution. Within the United States, it has been detected mainly in the Great Lakes region, including Michigan, Wisconsin, Illinois, Minnesota, Iowa, the Dakotas, and Nebraska.1 This can be explained by the close proximity of these areas to the Mississippi Flyway, which is the migratory route of many birds that can be hosts for the parasites.
The interesting fact is, the schistosomes that usually give rise to this condition are non-human species, meaning they do not usually infect humans. Their normal hosts are birds and other mammals. Mature parasite lays eggs in birds like ducks and geese, and mammals like raccoons. Through the feces of these aquatic animals, eggs reach the water. The eggs hatch and the undeveloped parasite enters a new host: a specific snail, to continue its life cycle. There they develop into cercaria and get released back into the water. Then they find new natural hosts, aquatic birds, and mammals, and the cycle repeats.
If they come into contact with human flesh, they can divert from this normal life cycle to give you the swimmer’s itch. The larvae, also known as cercaria of these schistosomes pierce the human skin. That is why it is given the name “cercarial” dermatitis. The cercariae die shortly afterward within the skin layer just deep to the outermost epidermis. The cercarial proteins that are left behind cause the hypersensitivity reaction, giving rise to the outward manifestation of an intensely itchy rash.
Symptoms
Olivier L. has conducted a study by intentional exposure of volunteers to disease-causing parasites, in order to document the outward appearance of the skin rash as it progressed.2 Initially there is a tingling sensation and a bit of itching as the cercaria enter the body by penetration of outer skin layers. It is called primary itching and lasts for one hour or more before subsiding. A tiny macule of 1-2 millimeters in diameter may appear at the site of penetration during this period. They appear as tiny flat red spots on your skin.

swimmer’s itch in the initial stage with tiny flat red spots on the skin
They go away in several hours and then are replaced by papules. These papules are small raised spots on your skin that are extremely itchy. This is called secondary itching and arises usually after 10 to 15 hours after the larvae pierce the skin. Sometimes there is diffuse reddening of the area instead of papules, and the area can get swollen especially if you scratch or rub the rash. Another important fact to identify swimmer’s itch is the location of the rash. Usually, it only appears in places where the skin was directly exposed to contaminated water, so the skin which was covered in swimwear would not have the rash. Sometimes papules get confluent and the entire area of the rash becomes elevated.
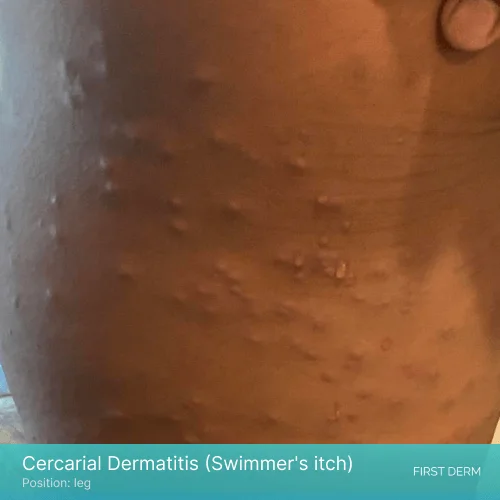
Cercarial dermatitis rash with papules and swelling on a leg
After these initial symptoms, papules can progress into blisters in two or three days. Vesicles form on the papules and they might rupture due to scratching or rubbing. This stage is accompanied by intermittent, irregular, and sporadic pruritus. It disappears in several days, and the rash itself disappears within a week after exposure to parasites if there are no secondary complications. Papules will be replaced by a pigmented spot that lasts for a few weeks upon healing.3 However, if the blisters rupture, the likelihood of secondary bacterial infection is more. This will lead to pustule formation and eruption.

Healing swimmer’s itch rash with pigmented skin
The same study shows how the initial exposure to parasites only give rise to mild symptoms, and secondary and subsequent exposures to the same parasite leads to more severe reaction.2 Therefore, the severity of cercarial dermatitis shows a direct connection to the number and the time duration of previous exposures to the same parasite.
And also, cases have been reported with persisting symptoms for about 20 days.4 Delayed appearance of the rash after 8 to 10 days from initial contact with the parasite is possible but rare. Also, it is not uncommon for an attack with a large number of cercariae to be accompanied by generalized symptoms such as nausea, fever, diarrhea, and swelling of lymph nodes and limbs.
Risk factors
Certain age groups and people who are doing certain occupations are more susceptible to the disease. Mentioned below are some high-risk populations.
- Children younger than 15 years of age who are more likely to play in shallow water areas.5 They are also less likely to follow any precautionary steps such as towel drying as soon as they come out of water.
- People who have occupational exposure E.g. Farmers/swimmers who are regularly exposed to water that may carry the parasite
- People with immunodeficiency
The risk of disease transmission is also linked with bathing behavior. Immersed activities such as swimming and wading are more risky than surface activities like surfing, boating and water skiing.5 Seasonal variation is also present because of high prevalence of snails in warm summer months.
Morning hours are high risk period of time during the day because that is when most of the cercariae emerge. As the day progresses, number of parasites in infected water reduces due to predation by other animals, therefore reducing the risk of human infection. Shallow water carries more cercariae than deep water. Also, if the water body is rich in aquatic vegetation, it is a potential high risk area and you better avoid taking a swim no matter how beautiful it looks.
Another thing to remember is, even if the water body has parasites, it would not remain that way forever. Factors like host presence can be subjected to change with time, and that can make the water safe again. However, there is no way to know whether it is safe or not, so always check for warning signs before you enter a shallow water area.
Diagnosis
Proper diagnosis of cercarial dermatitis is challenging because the rash can resemble many other disease conditions including insect bites, contact dermatitis and bacterial dermatitis. A history of recent contact with fresh or marine water bodies can be an indicator, and direct proof can be obtained by skin biopsy of papules within 48 hours of onset of them. For this, the doctor will shave off individual papules under local anesthesia, and the tissue would be examined under a microscope. In addition, laboratory tests will show increased eosinophil counts and increased total immunoglobulin E levels.6
As the rash disappears on its own in a week, you do not need to panic about it. Several methods of treatment are available to help you manage the symptoms, and to prevent secondary complications.
- Over-the-counter anti-itch creams and ointments such as calamine lotion and corticosteroid creams
- Cool compresses
- Prescription medications for severe cases E.g. oral antihistamines
- Antibiotics in case of secondary infection with bacteria
More than 70% of our users get better with Over-the-Counter Medication
When to see a healthcare provider?
Most of the time medical attention is not necessary. But if the rash persists for two weeks or more, it is better to go to a medical professional. And if there are pustules/ ruptured blisters/ extreme itchiness, your doctor will be able to prescribe you stronger medication to relieve you from the discomfort.
Prevention
The best method to avoid getting the swimmer’s itch is to block direct contact of skin with contaminated water. There are several preventive methods for this.
- Wearing protective clothing to cover the skin. E.g. wearing neoprene diving suits, rubber waders, and gloves is considered 100% reliable.3
- Applying waterproof sunscreen on exposed areas of skin before swimming.
- Avoid swimming/waddling in water bodies in areas with known snail or bird populations.
- Refrain from swimming in areas where cercarial dermatitis is a known problem.
If skin gets into contact with infected water, the number of cercaria piercing the skin can be minimized by several simple actions.
- Toweling the area
- Exposure of the area to sunlight immediately after coming out of the water
- Washing the area with 70% alcohol or soap and warm water in case of an accidental laboratory exposure
Reducing the parasites targeting the hosts (snails, aquatic birds) and the cercarial stage in water is another known method of prevention. Treatment of birds with anthelminthic drugs to kill the parasites, introducing “decoy snails” which are non-host snails for the target parasitic trematodes, and use of molluscicides to kill host snails and building traps for free cercariae in water are effective methods to achieve this target.5
Key points to remember
Cercarial dermatitis is an itchy rash with red macules, papules and swelling. You can get the disease if your skin is exposed to infected water with the microscopic parasite schistosomes, so the most reliable way to prevent spread is avoiding infected water. It does not spread from person to person. It is not a serious problem and normally does not require medical attention as it heals on its own in a short period of time. However, it is important to be aware of swimmer’s itch to avoid getting the disease and take preventive measures.
References
- Hoeffler DF. Cercarial dermatitis. Arch Environ Health. 1974;29(4):225-229. doi:10.1080/00039896.1974.10666573
- Olivier L. Schistosome dermatitis, a sensitization phenomenon. Am J Hyg. 1949;49(3):290-302. doi:10.1093/OXFORDJOURNALS.AJE.A119279
- Horák P, Mikeš L, Lichtenbergová L, Skála V, Soldánová M, Brant SV. Avian schistosomes and outbreaks of cercarial dermatitis. Clin Microbiol Rev. 2015;28(1):165-190. doi:10.1128/CMR.00043-14
- Kolářová L, Horák P, Skírnisson K, Marečková H, Doenhoff M. Cercarial dermatitis, a neglected allergic disease. Clin Rev Allergy Immunol. 2013;45(1):63-74. doi:10.1007/S12016-012-8334-Y
- Soldánová M, Selbach C, Kalbe M, Kostadinova A, Sures B. Swimmer’s itch: etiology, impact, and risk factors in Europe. Trends Parasitol. 2013;29(2):65-74. doi:10.1016/J.PT.2012.12.002
- Horák: Trichobilharzia – Google Scholar. Accessed April 15, 2023. https://scholar.google.com/scholar_lookup?title=Trichobilharzia&author=P+Horák&author=FM+Schets&author=L+Kolářová&author=SV+Brant&publication_year=2013&pages=455-465

The Specialist doctor from the University Hospital in Gothenburg, alumnus UC Berkeley. My doctoral dissertation is about Digital Health and I have published 5 scientific articles in teledermatology and artificial intelligence and others.






