Genital Warts – HPV (human papillomavirus)
Medically reviewed by The Dermatologists and written by Dr. Alexander Börve
Common
More than 200,000 US cases per year
- Transmitted through penetrative sex
- Requires medical diagnosis
- Symptoms: itching, burning, small bleeding, round raised warts
- Color: Typically skin-colored, pink to purple tinted
- Location: Genital area
- Treatment: podophyllotoxin, imiquimod, freezing (cryotherapy), electrosurgery (strong heating with electricity), laser, removal with scissors or knife
- Most genital warts recur within three months post-treatment
- Smoking heightens the risk of contracting genital warts
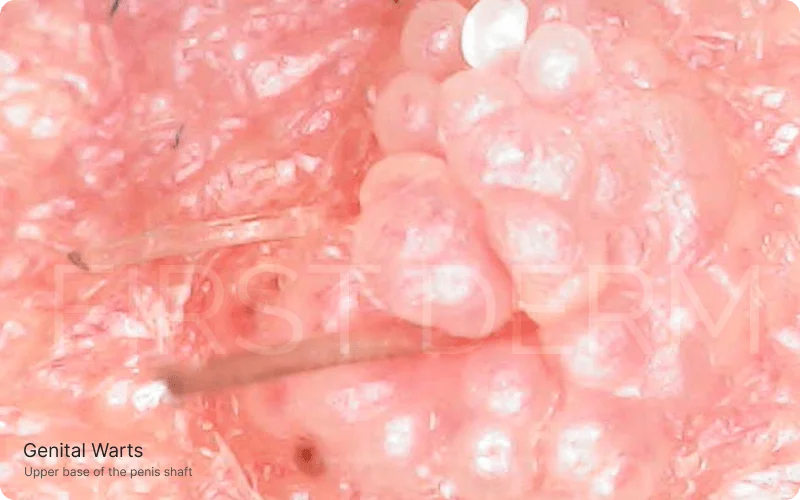
Magnified View of Genital Warts at the Upper Base of the Penis Shaft
Try our FREE dermatology search engine and get peace of mind within a second
Symptoms
Genital warts can appear on both the mucous membranes and the skin. They may look different and be in different places. The most common genital warts are lobe or round in shape and slightly raised. They are often skin-colored or pink to purple tinted, but may also be off-white, red or pigmented. You can have single warts, but usually several appear simultaneously. In some cases, the warts are located very close together so they may look like large single growths. Both women and men may experience itching, burning, small bleeding from the nipple and difficult intercourse if infected.
For men:
Genital Warts in the Pubic Area: Apart from the immediate genital area, warts can also manifest in the surrounding pubic region, sometimes blending in with the hair and being mistaken for other skin conditions.
![Genital Warts (01) pubic HPV (human papillomavirus) [ICD-10 A63.0]](https://firstderm.com/wp-content/uploads/Genital-Warts-02-skin-ICD-10-A63.0-1.jpg)
A detailed depiction of genital warts in the male pubic area, showcasing closely located individual blisters characterized by small, non-eruptive bumps.
Genital Warts at the Base of the Penis: The area where the penis meets the body is another location for these warts, which can be discreet but cause discomfort due to friction with clothing.
Detailed image showing genital warts located at the base of the penis
Blisters on the Foreskin Top: Warts can also present as blister-like formations, especially on the sensitive skin of the penis’s foreskin, potentially leading to additional discomfort during movements.
A close-up of blisters or wart-like formations on the foreskin top of the penis
Continuing on, genital warts for men are most common behind the penis, the glans, and the foreskin on the inside. Warts also occur on the shaft of the penis and around the anus even without having had anal intercourse. For women, the warts are common in all areas of the genital region, particularly the vaginal opening in the bottom part and of the labia minora. Sometimes, genital warts also appear on the outer labia, around the clitoris, the urethral meatus, in the upper part of the vagina, on the cervix, perineum, or around the anus.
You may have heard about getting “flat warts.” They are a virus altered mucosa that do not present as visible or noticeable warts. However, if a man is unable to see the warts on the penis or scrotum, it is rare that they exist. If the woman has symptoms of wart-like change, she may get an assessment from her healthcare provider. The physician usually uses a magnifying glass or special microscope to make it easier to diagnose.
The immune system plays a role in HPV infection. If the immune system is impaired (e.g. when you are pregnant), a viral infection can do more and more warts may form. However, these warts usually disappear when the mother’s immune system returns to normal after delivery.
Preventing and Managing Genital Warts
Most people who have genital warts get rid of warts, without any special treatment. It usually takes about a year, but it may also take longer. It is very unusual to still have warts when five years have passed from the time you are infected. If you have had genital warts during a period when the immune system was temporarily impaired, the warts usually reduce or disappear when the immune system recovers.
Condoms offer protection against genital warts, but it is not a full protection because the condom does not cover all surfaces that may be infected with viruses. There are also vaccines that protect you against the two types of HPV that are most common in genital warts and cervical cancer. The vaccine is more effective if you get them before you come into contact with these viruses. This reduces the likelihood of getting genital warts by 80 percent. Therefore, it is recommended that you get vaccinated before your first sexual intercourse. The vaccine has been shown to be effective in both sexes.
Try our FREE dermatology search engine and get peace of mind within a second
When to Seek Medical Advice for Genital Warts: Guidelines and STD Screening
If there are changes in the genital area, you contact your healthcare provider to investigate the possibility of sexually transmitted diseases (STDs). If an adult woman has not taken a Pap smear in the last two to three years, it may be helpful to get one. There are also tests to look for other STDs, such as chlamydia.
Sometimes the physician can also use the tissue sample. A small chunk of the changed skin will be removed after local anesthesia and be examined in a laboratory with microscopes to see if there are signs of a viral infection. This is usually unnecessary because most of the time doctors are able to see immediately if there are warts or not.
Genital warts do not directly lead to cervical cancer, so women who have had genital warts do not need to make any additional Pap smear checks. However, it is advised that all adult women get a Pap smear every three years. It is important to be examined by a gynecologist regularly, precisely because it can be difficult to differentiate warts from serious changes in the cervix. Sometimes genital warts are similar to changes in the cervix at a screening test.
The warts should be treated if you have symptoms such as itching, burning, bleeding and difficulty urinating. If you experience psychological disorders when you have genital warts, you should also get treatment.
If you are pregnant and have genital warts, the virus can be transmitted to the baby during birth in some cases. However, it is very rare that the child has any symptoms, but the virus could lie dormant, perhaps as long as several years, and later cause warts on the baby. Therefore, you should seek medical advice if you are pregnant and have genital warts.
Try our FREE dermatology search engine and get peace of mind within a second
Treatment for Genital Warts
There are several different ways to treat genital warts. Most focus on removing the warts, which does not treat the virus itself. Therefore, about a third get new warts after treatment. During a medical treatment or healing after a surgical treatment, you should not have sexual intercourse.
Treatment with solutions and creams can cause temporary problems with itching, burning, redness and minor injuries. In addition, it has been discussed whether women who have gone through repeated treatments for genital warts easier to get chronic pain in the vaginal opening, called vestibulitis. Therefore, it may be helpful to discuss with your doctor how to treat genital warts that do not disappear with treatment or recurring warts.
Treatment with podophyllotoxin
The most common treatment is with drugs containing podophyllotoxin, such as Wartec and Condyline. Wartec is also available as a cream, which can be easier to use especially for women. Treatment generally lasts three days, and then a break for about four days. After that, the treatment may be repeated one or more times. During the treatment, it is common to become red and get burning. If the reactions are overwhelming, the treatment should be discontinued. Most are completely well or significantly better within one month of treatment. If you are pregnant or planning pregnancy should not use Wartec or Condyline.
Treatment with imiquimod
Another substance used in severe cases is imiquimod. It stimulates the body’s immune system to take care of both the virus infection and the warts. Imiquimod may in the form of a cream, such as Aldara. The treatment takes longer on average (about two months) and costs more than treatment with podophyllotoxin. Imiquimod also creates side effect, such as redness, itching and burning. The treatment results in fewer recurrences than other methods.
Latest updates:
HPV Vaccine: A single dose Prevents Infection For At least Three years
Surgical Procedures for Genital Warts
- Freezing (cryotherapy)
- Electrosurgery (strong heating with electricity)
- Laser
- Removal with scissors or knife
Updated on November 08, 2023
Source
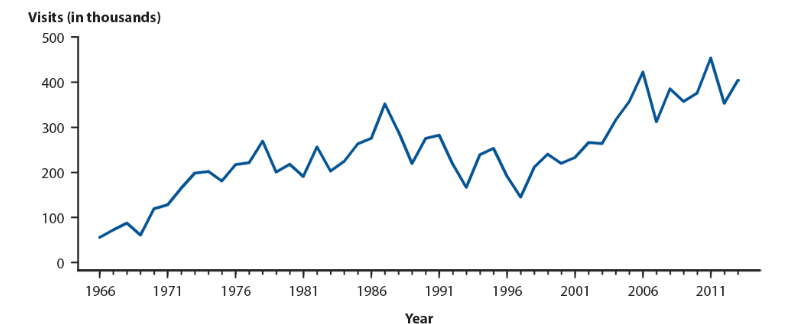
- Centers for Disease Control and Prevention. 2014 Sexually Transmitted Diseases Surveillance. Available at: http://www.cdc.gov/std/stats14/figures/50.htm
- American Academy of Dermatology. Genital warts: Diagnosis and treatment. AAD. Available from: https://www.aad.org/public/diseases/a-z/genital-warts-treatment
- Centers for Disease Control and Prevention. Human Papillomavirus (HPV), the Vaccine for HPV, and Cancers Caused by HPV. CDC. Published 2021. Accessed November 8, 2023. https://www.cdc.gov/hpv/index.html
- Leslie SW, Sajjad H, Kumar S. Genital Warts. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Updated 2023 May 30. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441884/
- National Cancer Institute. Human Papillomavirus (HPV) Vaccines. National Institutes of Health. Available from: https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-vaccine-fact-sheet
Ask a Dermatologist
Anonymous, fast and secure!

The Specialist doctor from the University Hospital in Gothenburg, alumnus UC Berkeley. My doctoral dissertation is about Digital Health and I have published 5 scientific articles in teledermatology and artificial intelligence and others.
![Genital Warts (02) HPV (human papillomavirus) penis [ICD-10 A63.0]](https://firstderm.com/wp-content/uploads/Genital-Warts-01-penis-ICD-10-A63.0-1.jpg)
![Genital Warts (04) HPV (human papillomavirus) penis [ICD-10 A63.0]](https://firstderm.com/wp-content/uploads/First-Derm-HPV-Genital-Warts-ICD-10-A63.jpg)