Genital Herpes
Medically reviewed by The Dermatologists and written by Dr. Alexander Börve
Genital herpes is caused by a contagious virus called herpes simplex. Herpes is a common skin disease that can be categorized into two categories: HSV-1 and HSV-2. Both types of herpes may present with symptoms of blisters or sores in the affected region. HSV-1 and HSV-2 are most commonly associated with outbreaks around mouth and genital area respectively, but either type may be found in either location. HSV-2 can also appear around the anus, on the buttocks and thighs, and thus is generally called genital herpes.
![Picture of Genital Herpes blisters [ICD-10 A60.0] - Genital herpes in women](https://firstderm.com/wp-content/uploads/Genital-Herpes-13-skin-ICD-10-A60.0.jpg)
Genital herpes in women: Characterized by ruptured blisters on the vulva, leaving distinctive scabs.
It is transmitted primarily through sexual intercourse or oral sex. Transmission of the virus usually occurs through direct skin-to-skin contact with the sores or secretions, even though transmission is possible even when these external symptoms are not present. The herpes virus is very sensitive and dies quickly outside the body. Therefore, you cannot be infected with genital herpes through contact with toilet seats, bath or towels.
Symptoms Genital Herpes
When the symptoms are visible, it is called a ‘herpes outbreak’. The herpes outbreak with symptoms may manifest itself by swelling, tenderness, pain and sometimes itching in the genital area. Transmission through oral sex can lead to herpes outbreak in the throat, which often causes very painful tonsillitis with similar symptoms. Anal intercourse can result in herpes breaking out around the anus.
![Picture of Genital Herpes (01) anus [ICD-10 A60.0]](https://firstderm.com/wp-content/uploads/Genital-Herpes-01-anus-ICD-10-A60.0-1.jpg)
Genital Herpes (ICD-10 A60.0) in the anal region: This image captures genital herpes, characterized by blisters and sores around the anus and buttocks
There are several stages of herpes outbreak. First, herpes blisters (also known as fever blisters or cold sores), appear as one or more blisters or watery sores in a group around the affected region. These blisters are usually smaller than 2 millimeters (about 0.08 in) in size. Then these blisters can rupture and give rise to painful ulcers or sores. The sores are typically inflamed and painful, and over the course of the outbreak, they can leak clear or yellowish fluid and leave a scab. They would be tender to touch.
There is a lot of variability in terms of the duration, appearance, and recurrence of herpes outbreaks. Most new cases are reported to show no symptoms at all, or symptoms that are short lived. [5] Some individuals, for instance, are unaware that they have the disease because their symptoms are so minor. Others, however, may have many outbreaks per year. Additional symptoms, most typical during the initial outbreak, may include fever, headache, body ache or fatigue. You might also notice swollen lymph nodes in the groin area. It takes only 2 to 12 days for the symptoms to appear after you get exposed to the virus.
![Picture of Genital Herpes visible symptoms on groin [ICD-10 A60.0]](https://firstderm.com/wp-content/uploads/Genital-Herpes-19-skin-ICD-10-A60.0.jpg)
Genital Herpes on Groin: Aftermath of herpes blisters rupturing, leaving behind shallow, painful ulcers. These reddish open sores are characteristic of a genital herpes outbreak, presenting as reddened areas in the groin
You might also experience painful urination and discharge from vagina or urethra if you are infected with herpes. And upon reactivation after the primary infection, herpes can cause damage to your nervous system, and can even cause serious conditions like meningitis and encephalitis.
The herpes virus does not disappear from the body after it has healed but remains throughout life. It rests in nerve cells next to the spinal cord and may be reactivated, giving new outbreaks of blisters and sores.
![Picture of Genital Herpes symptoms on male pubic region [ICD-10 A60.0]](https://firstderm.com/wp-content/uploads/Genital-Herpes-04-penis-ICD-10-A60.0.jpg)
Genital Herpes Symptoms on Male Pubic Region: Highlights visible blisters located at the base of the shaft, indicative of a genital herpes outbreak
Is it really genital herpes?
Genital herpes is not the only condition that causes bumps in pubic area. It is common to confuse c or genital warts with genital herpes. So, it is important to know the difference between these conditions because otherwise you are going to panic for no reason. Both ingrown hair and genital herpes cause tender small bumps that can rupture. The difference is herpes blisters are usually in clusters and reappear after healing, while ingrown hair is usually a single bump that does not return once healed.
Further Reading: Ingrown Hair Vs Herpes: Spotting the Differences
Genital warts are another condition you might confuse with herpes. It is caused by human papillomavirus. The blisters in genital warts are skin colored and appear as cauliflower tops compared to the herpes blisters.
But sometimes even trained doctors struggle to correctly identify which is which, so do not feel bad if you can’t tell the difference. To be sure of the diagnosis, doctors will do a blood test or a screening test for sexually transmitted diseases.
How does genital herpes spread?
Much like many skin diseases, it also spreads from close skin to skin contact. However, for herpes to spread, there should be prior damage in the normally seamless protective organ; skin.[3] These defects don’t have to be big. In fact, microscopic ruptures that happen during sex or abrasions of outermost layers of skin can provide a path for the virus to enter your body.
A surefire way to get herpes is sexual contact with an infected person. This includes vaginal, anal and oral sex. This is why genital herpes is most common among people between 16 to 40 years of age, which is the most sexually active age group.[3] When it comes to sexually transmitted diseases, one question most people have is; can it spread by kissing? Well, in this case the answer is yes. Especially the HSV-1, which gives rise to blisters mainly around the mouth, is known to spread in this manner. Then it can spread to genitals, causing genital herpes.

Genital Herpes in Women: Image depicts a reddish blister on the inner lips, a common symptom of a genital herpes outbreak
Studies have shown that almost 100% of sex workers are suffering from this condition, and female herpes is twice as much common than herpes in men in developing countries.[4]
Also, genital herpes is more likely to spread during the outbreaks, when the symptoms are visible, and the virus is actually on the surface of the skin of the infected person. Even though less strong, this virus also spreads during the period where there are no symptoms.
Female herpes and pregnancy
Herpes does not affect the ability to get pregnant, but in connection with childbirth, there is a small risk of transmitting herpes to the newborn child, who can then become very sick. The risk is greatest when you have herpes for the first time and if you were infected during the latter part of the pregnancy. If you have had herpes since before getting pregnant, your body will produce and deliver certain antibodies to the baby, which will help shield it from the virus. So, it is important to consult your doctor if you suspect that you have received a herpes outbreak during late pregnancy.
While there is a risk of spreading the disease to the newborn during childbirth, it is also possible that you might give birth to a healthy child. The important question is, if you have herpes and you are pregnant, should you continue to take herpes medication?
Since we all have heard how drugs can affect the child inside your womb, it is only natural to be reluctant to take more medicine than what is absolutely necessary. However, studies have shown a bigger risk of premature childbirth if you discontinue treatment during pregnancy.[6] Also, many anti-herpes drugs such as oral acyclovir and valacyclovir are proven to reduce the likelihood of infection to the newborn, without compromising the safety of the fetus.[6] So, you should definitely continue the anti-herpes treatment during pregnancy. And if there is a herpes outbreak at the time of labor, you might want to consider cesarian section instead of normal vaginal delivery, as it minimizes the disease transmission to the baby.
When should I seek medical care?
While it is very rare, you can get bacteria in the wounds that are formed when herpes blisters burst. In addition, an unusual complication can occur the first time you get herpes. You will have mild meningitis, and then get severe headaches and stiff neck. In both cases, you should contact your healthcare provider. And of course, if you are pregnant, it is important to inform the doctor about STI for the protection of the baby.
Once you visit your doctor, he will make a diagnosis after inspecting the blisters in the affected area and the history of recent sexual activity. To confirm the diagnosis, he might collect a sample from one of the active sores. This sample will be tested for the presence or absence of the herpes virus.
You can read more about how to get tested for and if you have genital herpes here
Treatment
At this time there is no known cure for either type of herpes, although there are treatments that suppress symptoms and reduce the possibility of the disease spreading. Your health care provider will recommend to you the best mode of treatment based on the type of HSV you are infected with, the severity of it and other medical factors.
Antiviral creams containing acyclovir (e.g. Zovirax) may relieve superficial symptoms. In some cases, when symptoms are severe, treatment with prescription antiviral medicine in tablet form may be required. It is not curative but suppresses the symptoms. In these cases, treatment should start as early as possible after the first signs of disease.
Home remedies
There are several things you can try at home to reduce the symptoms and relieve the pain. Salt baths, cold compression with ice packets to the affected area and over the counter pain relieving medicine such as paracetamol are some of those options. Remember, these won’t cure your herpes. It will only help reduce the symptoms.
What can I do?
The best way to reduce the risk of genital herpes infection is to use a condom during sexual intercourse, because those who are infected often do not know about it. However, condoms do not offer 100% protection because they do not cover the genitals entirely. Also, using a good silicon-based lubricant along with the condom, especially during anal sex can protect your skin from getting miniature abrasions, which will reduce the likelihood of disease transmission.
If you have on-going herpes outbreak with blisters, you should completely refrain from having unprotected sex because the risk of infection is greatest then. Taking known antiviral drugs before sexual intercourse with someone who is infected with herpes do not provide 100 percent protection.
All in all, the best precaution to take is to have a single long-time sexual partner who is tested negative for sexually transmitted diseases.
If you suspect you have genital herpes rather than living in doubt and fear, go to your doctor and get a closure to the problem. If you are infected, take your medicine properly, and you will be able to live a fairly normal life.
Finally, if you have only recently found out you have genital herpes, have done the online research and scared to death because of what you’ve seen and read, you should calm down. Despite the huge amount of social stigma surrounding genital herpes, it is not as bad as it sounds. The worst thing you have to do might be breaking the news to your current or future sexual partner/s.
Ask a Dermatologist
Anonymous, fast and secure!
References
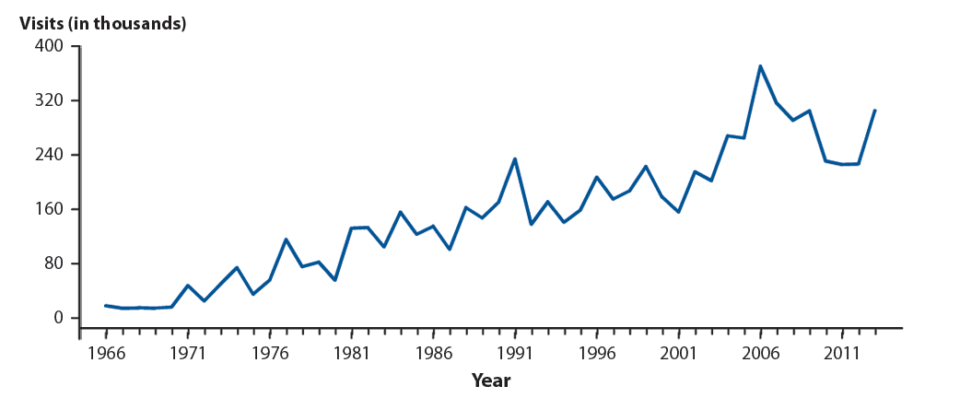
- National Disease and Therapeutic Index, IMS Health, Integrated Promotional Services™. IMS Health Report, 1966–2013. Available at: http://www.cdc.gov/std/stats14/figures/53.htm
- Time Trends in First Episode Genital Herpes Simplex Virus Infections in an Urban STD Clinic. Dabestani N, Katz DA, Dombrowski J, Magaret A, Wald A, Johnston C. Sex Transm Dis. 2019 Oct 30.
- Zhu S, Viejo-Borbolla A. Pathogenesis and virulence of herpes simplex virus. Virulence. 2021 Dec;12(1):2670-2702. doi: 10.1080/21505594.2021.1982373. PMID: 34676800; PMCID: PMC8923070.
- Looker, K. J., Johnston, C., Welton, N. J., James, C., Vickerman, P., Turner, K. M. E., Boily, M. C., & Gottlieb, S. L. (2020). The global and regional burden of genital ulcer disease due to herpes simplex virus: a natural history modelling study. BMJ Global Health, 5(3). https://doi.org/10.1136/BMJGH-2019-001875
- Garland, S. M., & Steben, M. (2014). Genital herpes. Best Practice & Research. Clinical Obstetrics & Gynaecology, 28(7), 1098–1110. https://doi.org/10.1016/J.BPOBGYN.2014.07.015
- Safety of antiviral medication for the treatment of herpes during pregnancy – PubMed. (n.d.). Retrieved January 24, 2023, from https://pubmed.ncbi.nlm.nih.gov/21490353/

The Specialist doctor from the University Hospital in Gothenburg, alumnus UC Berkeley. My doctoral dissertation is about Digital Health and I have published 5 scientific articles in teledermatology and artificial intelligence and others.